-

Using Big Data Approaches to Map Myocardial Infarction Signatures
Aisha Y. Abdool, Merry L. Lindsey, and Upendra Chalise
Myocardial Infarction (MI) results in a loss of cardiomyocytes, which stimulates a wound healing response to form scar tissue in the heart. Mapping inflammatory and extracellular matrix (ECM) gene changes after MI will help us to understand the temporal evolution in profiles. Using the Mouse Heart Attack Research Tool (mHART), a comprehensive database of previous MI studies in wild-type C57/BL6J mice, we retrospectively analyzed gene array data that included 84 inflammatory genes (n=91 mice) and 84 ECM genes (n=109 mice) at time 0 (no MI) and MI day (D)1, 3, 5, 7, and 28. Temporal evolution was assessed by ANOVA, and unpaired t-test was used to compare consecutive days. Ingenuity Pathway Analysis was used for data visualization and to identify pathways enriched at specific MI days. Overall, we saw three major shifts in wound healing after MI. The first was an early robust inflammation at D1 and D3, shifting to resolution of inflammation by D5 and D7, and leading to establishment of a neo-homeostasis by MI D28. The major genes represented at MI D1 were IL1b, IL1a, and IFNg; at D3 were inhibition of IL13, IL4, and C3; at D5 were activation of TGFb1, IFNg, and TNF; at D7 were inhibition of TNF, IL17Ra and IL36A; and at D28 inhibition of IFNg, CCR5, and CCR2. The transition from D0 to MI D1 showed maximum activation of the inflammatory response, with the primary pathways induced being activation and adhesion of neutrophils, cellular movement, and recruitment of antigen presenting cells. The signaling pathways induced during the shift from MI D5 to D7 included inhibition of cellular infiltration of myeloid cells and inhibition of chemotaxis of monocytes. Pathways induced from MI D7 to D28 indicated a shift to the new homeostasis indicated by further inhibition of cellular movement and inhibition of growth of blood vessels. In summary, our evaluation revealed a steady shift in signaling from early inflammation to resolution and repair over the course of MI.
-

Updating and Validating the Rheumatic Disease Comorbidity Index to ICD-10-CM
Hanifah Ali, Punyasha Roul, Yangyuna Yang, Kaleb Michaud, Ted R. Mikuls, and Bryant England
Background/Objective: Comorbidities can contribute to increased risk for mortality and disability in individuals with rheumatoid arthritis (RA)1,2. The Rheumatic Disease Comorbidity Index (RDCI) assesses 11 comorbidities and produces a weighted score (0-9) that accurately predicts several health outcomes3. The RDCI was developed with self-report data and later validated with ICD-9-CM codes collected from administrative data3,4. On October 1, 2015, the U.S. transitioned to ICD-10-CM, resulting in a nearly five-fold increase in the number of codes available to classify conditions5. Our objective was to update the RDCI by translating it into ICD-10-CM.
Methods: We defined an ICD-9-CM cohort and an ICD-10-CM cohort using patient data from the Veterans Affairs Rheumatoid Arthritis Registry (VARA). ICD-10-CM codes were generated by converting ICD-9-CM codes using tools that provide suggested crosswalks, and the codes were reviewed by a physician to assess clinical relevance. Comorbidities were collected from national VA administrative data over a two-year period in both cohorts (ICD-9-CM: October 1, 2013 to September 30, 2015; ICD-10-CM: January 1, 2016 to December 31, 2017). Comorbidity frequencies were compared using Cohen’s Kappa, and RDCI scores were compared using Intraclass Correlation Coefficients (ICC).
Results: Both the ICD-9-CM cohort (n=1,082) and ICD-10-CM cohort (n=1,446) were predominantly male (ICD-9-CM: 89%; ICD-10-CM: 87%), Caucasian (ICD-9-CM: 76%; ICD-10-CM: 73%), and middle to old-aged (ICD-9-CM: 67.3 ± 10.2 years; ICD-10-CM: 68.2 ± 10.0 years). Prevalence of comorbidities were similar between coding systems, with absolute differences less than 4% (range: 0.28 to 3.91). Myocardial infarction, hypertension, diabetes mellitus, depression, stroke, other cardiovascular, lung disease, and cancer had moderate agreement or higher (range κ: 0.47 to 0.84), while fracture and ulcer/stomach problem had slight and fair agreement, respectively (κ = 0.13; κ = 0.27)6,7. The RDCI scores were 2.95 ± 1.73 (mean ± SD) for the ICD-9-CM cohort and 2.93 ± 1.75 for the ICD-10-CM cohort. RDCI scores had moderate agreement (ICC: 0.71; 95% CI: 0.68-0.74)8 among individuals who were observed during both the ICD-9-CM and ICD-10-CM eras.
Conclusion: We have mapped the RDCI from ICD-9-CM to ICD-10-CM codes, generating comparable RDCI scores in a large RA registry. Individual comorbidity agreement varied, with more chronic conditions such as diabetes and hypertension having higher agreement and more acute conditions such as fractures and ulcer/stomach problems having lower agreement. The updated RDCI can be used in clinical outcomes research with ICD-10-CM era patient data.
-

Differences in Maternal and Infant Cord Blood Vitamin D Between Racial/Ethnic Groups
Khadijjta Y. Ali, Matthew VanOrmer, Melissa Thoene, Maranda Thompson, Rebecca Slotkowski, Ridhi Chaudhary, Nicole Bender, Alyssa Freeman, Alexandra Hergenrader, Olivia Paetz, Sarah Sweeney, Corrine Hanson, and Ann Anderson-Berry
Background: Vitamin D deficiency associated with lower 25-hydroxyvitamin D (25(OH)D) concentration is common among individuals with more melanin pigmentation. Low 25(OH)D levels in pregnant women may be related to increased risk of low birth weight and preterm delivery. Still, few studies have assessed how serum levels of 25(OH)D vary between maternal and infant race/ethnicity.
Objective: This study aimed to investigate the relationship between 25(OH)D levels in maternal blood and infant cord blood within certain ethnic groups, prematurity status, and low birth weight.
Experimental Design:An IRB-approved study enrolled 86 mother-infant pairs. Maternal blood samples and infant cord blood samples were analyzed for 25(OH)D serum levels. Descriptive statistics and Kruskal-Willis tests comparisons were conducted with the use of IBM SPSS Statistics 28 software to assess the relationship between maternal and cord blood 25(OH)D levels in other race/ethnicity groups, birthweight, and preterm birth. Prematurity was categorized into two groups: premature (weeks) and term (≥37 weeks). Birth weight was categorized into two groups: low birth weight (< 2500 g weeks) and not low birth weight (≥2500 g weeks). A p-value of
Results:Median levels of 25(OH)D serum were lower in infant’s cord blood (22.52 ng/mL) than maternal blood (38.06 ng/mL). White participants had significantly higher 25(OH)D levels than African American participants in both maternal blood (40.76 ng/mL vs 27.79, p =
Conclusion: Our findings suggest a possible association with lower serum 25-hydroxyvitamin D concentration in darker skin pigmentation, even in a small sample size. These results suggest that prematurity and birth weight should be replicated in larger sample sizes of different Race/Ethnic groups, limiting this finding. Further studies should focus on examining differences with larger and more diverse sample sizes. Such research should include measuring Vitamin D intake in pregnancy and clinical outcomes.
-
Assessing Maternal Dietary Iodine Intake During Pregnancy and its Effect on Infant Birth Growth Outcomes
Nicole S. Bender
Iodine is an essential micronutrient that must be obtained through dietary sources such as dairy products, fish, and iodized salt. Iodine plays an important role in the function of the thyroid and its ability to produce triiodothyronine (T3) and thyroxine (T4). The thyroid is involved in fetal neurocognitive development and metabolism. The objective of this study was to assess whether maternal dietary iodine intake during pregnancy affects birth anthropometrics and gestation length in infants. This study enrolled 46 mother-infant pairs at the time of delivery for sample collection and completion of a dietary intake assessment. Only one mother was found to be adequate for dietary iodine intake. The results showed a significant correlation between birth length percentile and iodine intake. Severe maternal iodine deficiency can lead to congenital hypothyroidism and goiter in neonates, reflecting the importance of sufficient iodine intake during pregnancy. Future directions include enrolling a larger sample size and considering use of a different nutritional assessment tool. Understanding the impact of iodine deficiency during pregnancy may be crucial to improving patient outcomes in this vulnerable population.
-

Comparison of Nucleic Acid Extraction Kits for Detecting Pathogens in Spiked Human Serum
Kate Berzonsky, Catherine Pratt, Bailey White, Dylan George, and Mike Wiley PhD
Nucleic acid extraction is a laboratory process by which DNA and RNA can be isolated for downstream applications. Currently, there are many commercial DNA and RNA extraction kits available to simplify this process. These kits vary in cost, processing time, and required materials. While most studies comparing commercial extraction kits analyze using real-time qPCR, DNA sequencing has become a popular technique for determining specific pathogens present in microbial communities. This study compares the ability of 11 different nucleic extraction kits to detect pathogens from samples spiked with known proportions of bacteria and yeast. Additionally, variations of the kits were performed, including different lysis techniques or addition of carrier RNA. Ultimately, the results of the study demonstrate that the use of mechanical or enzyme-based lysis techniques generally result in proportions that are more accurate to that of the known standard. Taking into consideration the required materials for each kit, some kits can also be identified as effective options for low-resource environments.
-
Outcomes Of Pulmonary Valve Replacement in Adult Congenital Heart Disease
Madison R. Bezousek
Congenital cardiac diseases involving the pulmonary valve are some of the most common forms of congenital heart disease. Over 85% of patients with CHD now live into adulthood making PVR (pulmonary valve replacement) one of the most ACHD procedures. Outcomes of PVR are well established but can differ by institution which is why it was important to assess our institution to compare to national averages. There are two forms of pulmonary valve replacement: Surgical PVR has been the standard of care for the last several decades. Bioprosthetic valves are traditionally placed through an open sternotomy under cardiopulmonary bypass. Outcomes are generally excellent. Valves vary in structure and make-up, but generally last 10 or more years. Catheter based pulmonary valves have been in existence since the mid 2000s and within our program since early 2010s. Valves are placed under fluoroscopic guidance most commonly within a pre-existing surgically placed valve. Outcomes are generally excellent and have similar outcomes to surgical pulmonary valves.Catheter based PVR for native pulmonary valve disease will soon be available (Harmony) and establishing both surgical and catheter based pulmonary valve replacement will be important for future decision making.
The objectives of this study were to investigate pulmonary valve durability and outcomes in adults seen by the pediatric and adult congenital heart disease program at Children’s Hospital and Nebraska Medicine over since the advent of catheter based PVR. Compare indications and medical comorbidities for patients that undergo a surgical pulmonary valve replacement to those that receive a catheterization procedure.Assess and compare pre- and post-operative statuses of the patients receiving pulmonary valve replacement.
IRB approval was achieved for this study which consisted of retrospective cross-sectional chart review with the Inclusion criteria: ACHD patients ≥18 years who underwent pulmonary valvereplacement either through surgical or catheterization intervention in the last 10 years. Patients were reviewed and described. Valve longevity, endocarditis, extubated in the operating room, reoperation, readmittance, and complications were assessed. Duration is calculated using the day of the valve replacement and the last known clinic date. Pulmonary stenosis, pulmonary regurgitation, and mixed valve disease are indicated using Echocardiograms and Cardiac MRI’s when present at the clinic date prior to the procedure and the most recent cardiac clinic date. From this research it is concluded that Surgical PVR are highly successful with low mortality rates, low valve failures, and generally short hospital length of stay. Procedural complications are low and valve failure is rare. Catheterization procedures are also highly successful and have a significantly shorter length of stay, have a higher extubated in the operating room rate, low mortality rate, and low valve failure. Endocarditis has been previously published as higher for catheterization PVRs but for this institution the endocarditis rate is low for both surgical and catheterization. Catheterization pulmonary valve replacement is proven to be effective and should be used as the 1st recommendation for those that qualify for that type of intervention.
-

"CHRI"sis at the NICU: The Medley with Midazolam
Reeyan Bhakat, Nghi M. Nguyen, Victoria L. Schaal, and Gurudutt Pendyala
Approximately 1.5 million neonates undergo anesthesia for surgical procedures in the United States every year1. Midazolam is a commonly used anesthetic agent used in the Neonatal Intensive Care Unit (NICU). It is used to sedate neonates and facilitates complex procedures such as mechanical ventilation.2 The extensive use of midazolam has raised questions about whether it affects the cognitive development of infants. In 2014, the International Anesthesia Research Society released a statement saying, “Surgeries and procedures requiring anesthetic and sedative drugs that could reasonably be delayed should possibly be postponed because of the potential risk to the developing brain of infants, toddlers, and preschool children”. 3 Although some evidence shows that midazolam exposure could harm an infant’s cognitive development, little is known about what parts of the developing brain are directly affected by midazolam. Additionally, research has yet to uncover whether the effects of midazolam persist into adulthood. In order to examine the consequences of midazolam exposure, a holistic system biology approach should be implemented. Experimental data from four different levels ─ the molecular level, the physical trait level, the behavioral level, and “omics” level would help address these issues. Our objective is to investigate how prolonged exposure to midazolam affects cellular as well as behavioral functions. A rodent model was implemented to study the effects at infanthood, adolescence, and adulthood. Our molecular results revealed that midazolam could potentially cause disturbances in key brain protein levels. Additionally, midazolam could potentially contribute to social deficits as evidenced by behavioral results. Overall, the results all point to midazolam's potential to delay proper neurodevelopment.
-
Impact of COVID-19 Infection During Pregnancy on Neonatal Birth Outcomes
Ridhi Chaudhary, Melissa Thoene, Matthew Van Ormer, Maranda Thompson, Rebecca Slotkowski, Nicole S. Bender, Khadijjta Y. Ali, Alyssa Freeman, Alexandra Hergenrader, Sarah A. Sweeney, Olivia R. Paetz, Corrine K. Hanson, and Ann Anderson-Berry
Approximately 116 million births have been reported worldwide in the nine months following the start of the COVID-19 pandemic. Currently, the effects of COVID-19 infection during pregnancy on birth outcomes are not fully understood. An IRB-approved study enrolled 115 mothers since March 2020, 5 of whom had a confirmed history of COVID-19 infection during pregnancy. For each COVID-19-infected mother, two mothers of similar age, gestation period, and race who were not infected with COVID-19 during pregnancy were matched 2-to-1 for a case-control analysis. Descriptive statistics were generated, and the Mann-Whitney U test was used to compare continuous variables between the two groups. Fisher’s Exact test was used to evaluate categorical outcomes between the groups. P
-
Dissolvable microneedles and nanofiber dressings to eradicate biofilms and improve wound care
Jenna Cusick, Jingwei Xie, and Yajuan Su
Biofilms are communities of microorganisms consisting of one or more bacterial species that attach to a biotic or abiotic surface. Biofilms are highly common in chronic wounds. To improve wound care treatment, a Janus-type antimicrobial dressing was created to eradicate biofilms in chronic wounds. The dressing consists of two layers: a top layer of electrospun nanofibers and a bottom layer of dissolvable microneedles. The dressings were tested on an ex vivo and in vivo model.
-

TDP-43 Phase Separation Does Not Likely Regulate LPS-Induced Neuroinflammation
Marshall Dawkins, Justin Dunn, Ju Gao, Ariele Peters, Xiaojia Ren, Devanshi Shukla, Luwen Wang, and Xinglong Wang
Immunohistochemistry (IHC) was performed to assess whether Transactive response Deoxyribonucleic acid binding Protein 43 (TDP-43) liquid-liquid phase separation (LLPS) regulates lipopolysaccaride (LPS)-induced neuroinflammation. Quantification and intensity results of glia cells and cytokines indicate that TDP-43 LLPS does not likely regulate LPS-induced neuroinflammation.
-

Evidence for a Role of GluN2C/GluN2D-Containing NMDA Receptors in Neuronal Oscillations
John Doran, Tyler Miller, Kiran Sapkota, and Daniel T. Monaghan
Synchronization of neuronal firing leads to neural oscillations (brain waves) which are critical to working memory, cognition, and perception. NMDA receptors (NMDARs) play a vital role in establishing appropriate neural oscillations and modulating brain activity. Abnormalities in NMDARs have been linked to diseases such as schizophrenia causing impairments in working memory, cognition, and perception, which is thought to be due to abnormal brain wave patterns. Consistent with this hypothesis, general NMDA receptor blockers produce exaggerated neuronal oscillations and schizophrenia-like symptoms. Several NMDAR subtypes exist, and novel disease treatments may depend on targeting a select group of NMDAR subtypes. The drug UBP791 is a competitive antagonist that has a higher binding affinity for GluN2C/2D over GluN2A/2B. The selectivity of UBP791 allows for discrimination between these receptor subtypes and identifying the role of various NMDARs.
-

Pancreatic Enzyme Dosing and Gastrointestinal Symptoms in Children with Cystic Fibrosis
Lauren Dreyer and Heather Thomas
The aim of this study is to determine if higher than the recommended dosing for pancreatic enzyme replacement therapy (PERT) improves GI symptoms in children with Cystic fibrosis. Children with CF and exocrine pancreatic insufficiency (EPI) were categorized into two groups based on PERT dosing: less than 10,000 lipase units/kg/day, or greater than 10,000 lipase units/kg/day.
Methods:
142 pediatric CF patients from the Nebraska Regional CF Center were included in the retrospective evaluation. Patients were split into two different groups based on their pancreatic enzyme dosing. Group 1 was greater than 10,000 lipase units/kg/day of enzymes, and group 2 was less than 10,000 lipase units/kg/day.
Results:
The p-value of the results was 0.5992, meaning that there was no statistical difference between the GI symptoms for those who take less or greater than 10,000 lipase units/kg/day of enzymes. The group that takes greater than 10,000 lipase units/kg/day are 1.194 times more likely to experience GI symptoms compared to the group with less than 10,000 lipase units per day.
Conclusion:
Based on the analysis that was completed on the data, there is no statistical significance between those that take greater or less than 10,000 lipase units/kg/day of pancreatic enzymes.
-

Large-scale Preclinical Swine Study Using Engineered Hemostatic Nanofiber Objects for the Treatment of Junctional Hemorrhage; Nanofiber Microspheres for Directing Cellular Growth and Response
Justin S. Dyke, Johnson Vitharikunnil John, and Jingwei Xie
This poster explores the use hemostatic nanofiber objects for treatment of non-compressible junctional hemorrhages by creating internal compression. Building upon previous studies changes were made to the method of producing nanofiber objects that is convertible to large-scale production. This poster also explores the use of nanofiber microspheres for tissue repair and regenerative applications. Two methods were explored in the use of electrospraying with and without adding air to the solution to adjust porosity of the microspheres. Both studies contained the use of electrospinning nanofibers and crosslinking of materials to adjust desired properties.
-

Sleep Disordered Breathing Screening in Hospitalized Patients with COPD Using Overnight Oximetry and End-Tidal Carbon Dioxide Monitoring: A Feasibility Study
Katherine E. Erwin and Jennifer N. Miller
Chronic obstructive pulmonary disease (COPD) and sleep apnea are overlap syndromes and cause an increased systemic inflammatory response, a weakened immune system, poor cognition, and physical inactivity in addition to COPD patients’ comorbid factors causing an overall decreased functional status. Feasibility testing of physiologic measures is needed to promote more accurate screening of sleep-disordered breathing in patients with COPD. This study hypothesizes more effective screening with utilization of overnight oximetry and end-tidal carbon dioxide level monitoring to detect sleep-disordered breathing. This descriptive study will test the feasibility of completing OSA and central sleep apnea screening in hospitalized patients with COPD who have not been diagnosed with a sleep-related breathing disorder. The aim of this study is to evaluate the feasibility of study a) enrollment (recruitment, efficiency, attrition, problems), b) data collection (technology transfer of data, instruments, time required, missing data), and c) clinical data collection from electronic medical record (inpatient and private practice settings). The Chronic Disease Self-Management Theory by Dr. Katie Lorig was utilized as the theoretical framework for this study to incorporate self-management in treatment of these two chronic disorders. This study looks at participants (N=10) who were recruited from Bryan Health in Lincoln, NE and followed post-discharge at Nebraska Pulmonary Specialties, LLC. Following completion of self-reported measures, patients will have overnight oximetry and end-tidal CO2 measured 1-2 days prior to discharge. Study information will be given to their providers at Nebraska Pulmonary Specialties and sleep study data will be obtained if ordered. Descriptive statistics will be completed to evaluate the feasibility of the study after completion. Recruitment and enrollment are underway and results are pending.
-
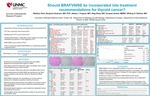
Should BRAFV600E be Incorporated into Treatment Recommendations for Thyroid Cancer?
Madelyn R. Fitch; Whitney S. Goldner MD; Benjamin Swanson MD, PhD; Abbey L. Fingeret MD; Oleg Shats MS; and Anupam Kotwal MBBS
Around 90% of all well-differentiated thyroid cancers are papillary thyroid carcinomas (PTC). PTCs have a recurrence rate of around 20% and a low mortality rate of around 5%. Within PTCs, around 60% of them have the BRAFV600E mutation. Currently, there is a debate on whether BRAFV600E is an independent predictor of tumor aggressiveness and recurrence. This study looks at whether BRAFV600E is an independent predictor of recurrence and outcomes in PTC. Tissue microarrays (TMA) were made from well-differentiated thyroid tumors and stained for the BRAFV600E mutation. BRAFV600E expression was calculated using an H-score: the staining intensity (0-3) multiplied by the amount of tumor that stained positive. A univariate analysis showed that BRAFV600E was significantly associated with age (p=0.0259), gender (p=0.019), extrathyroidal extension (p=0.049), positive margins (p=0.033), lymph node ratio (p=0.0106), N stage (p=0.015), AJCC 8 stage (p=0.0042), ATA risk category (p=0.018), and time to recurrence (p=0.0487). A multivariable analysis found that only extrathyroidal extension was an independent predictor of recurrence. Overall, BRAFV600E was not an independent predictor of recurrence in this cohort. Current treatment plans based on risk of recurrence appear to be appropriate, and it is not recommended that BRAFV600E be included as an independent variable.
-

Synthesis and Characterization of a Long-Acting Tenofovir ProTide Nanoformulation
Franchesca G. Fonseca, Srijanee Das, Denise Cobb, Mohammad U. Nayan, Howard E. Gendelman, and Benson Edagwa
Antiretroviral therapy (ART) has significantly improved the quality of life of Human Immunodeficiency Virus (HIV) patients; but adverse side effects and poor patient compliance to lifelong daily pills remain major challenges. To this end, the need for long acting (LA) therapies that can improve treatment adherence, positively affect drug resistance patterns in addition to limiting drug toxicities cannot be overstated. Tenofovir alafenamide (TAF), a nucleotide reverse transcriptase inhibitor of HIV infection and prodrug of tenofovir (TFV), is characterized by potent antiretroviral activities and high genetic barrier to viral resistance making it a suitable candidate for long-acting antiretroviral therapy. However, the inherent physicochemical features of TAF that includes high water solubility and susceptibility to degradation in aqueous buffers has limited its transformation into long-acting sustained release formulations. With these limitations in mind, this work sought to produce a stable TFV prodrug that would facilitate development of a long-acting formulation without compromising on TAF’s antiretroviral activity and safety profile. A lipophilic and hydrophobic prodrug of TFV (M1TFV) was therefore developed through chemical synthesis making it possible to formulate the drug as a stable aqueous nanosuspension to improve upon drug dissolution. The aqueous poloxamer stabilized TFV prodrug nanosuspension (NM1TFV) was characterized for physicochemical properties, chemical stability, cellular drug uptake and retention. The average particle size of the nanoparticles was 220-270 nm with a polydispersity index of
-

Non-Destructive Characterization of Peripheral Arteries using Intravascular Ultrasound
Colman Isaac Freel, Courtney Keiser, Majid Jadidi, Sylvie Sim, Yury Salkovskiy, Kaspars Maleckis, Anastasia Desyatova, Alexey Kamenskiy, and Jason MacTaggart
Peripheral Artery Disease (PAD) is the chronic obstruction of blood flow to the extremities caused by plaque buildup. Poor circulation results in exertional pain, numbness, and weakness, and in severe cases, can manifest critical conditions, including gangrene and limb loss. PAD affects approximately 8.5 million Americans and costs the United States $21 billion annually in direct medical expenses. High expenditures are attributed to operation and intervention failures resulting in frequent need for revascularization. Treatment of PAD typically involves lifestyle/diet adjustments, bypass surgery, or angioplasty/stenting. Unfortunately, repeated limb deformation during locomotion often results in adverse repair device-artery interactions, which hinder the long-term efficacy of endovascular therapies. Patient and lesion-specific device selection guided by computational modeling can help improve clinical outcomes, but these models rely heavily on accurately recorded three-dimensional arterial geometry and plaque composition. Intravascular ultrasound (IVUS) is a minimally invasive method of endovascular imaging that allows evaluation of the geometry and composition of the arterial wall, but its two-dimensional nature is often insufficient to capture complex three-dimensional plaques. We have developed a method of obtaining three-dimensional arterial geometry from two-dimensional IVUS images to build Computer-Aided Design models of calcified human femoropopliteal arteries. Our imaging method will allow for the characterization of calcium, necrotic core, fibrofatty, and fibrous tissue using IVUS. Correlation of IVUS images with conventional histology, micro-CT imaging, and clinical CTA data will help inform computational models.
-

Associations of Budd-Chiari Syndrome and Factors Predicting Need for TIPS and Liver Transplantation: Long-Term Single-Center Experience
Anusha L. Gopalam, Valerie K. Shostrom, Vijaya R. Bhatt, Alex B. Nester, Laxmi Narayana Buddharaju, Marco A. Olivera, and Krishna Gundabolu
Background: Budd-Chiari Syndrome (BCS) is a rare thrombotic disorder that involves obstruction of hepatic venous outflow. It can result in increased sinusoidal pressure and portal hypertension. Patients may develop cirrhosis and liver failure from chronic injury, along with other complications such as ascites and varices. BCS is associated with thrombophilia and hematological disorders such as myeloproliferative neoplasms (MPNs) and other auto-immune diseases. Patients typically receive long-term anticoagulation to decrease the risk of recurrence of thrombosis along with supportive measures such as trans-jugular intrahepatic portosystemic shunt (TIPS) and liver transplant.
Methods: We performed a retrospective study to describe the patient population with BCS at UNMC. We evaluated 23 patient medical records and collected data on demographics, risk factors, health history, BCS presentation, associated diseases, any acquired/inherited thrombophilia, laboratory results at the earliest available date from diagnosis, and treatments/procedures received. Model of End-Stage Liver Disease (MELD) and Child-Pugh scores were calculated and reported.
Descriptive Findings: The median age for the 23 patients in our study was 36 years (range: 11-59 years). The percentage of females was 60.87%. The overall survival rate was 91.3%. Median follow-up duration was 89 months (range: 3-330 months). Of the total, 57% of the patients had myeloproliferative neoplasms (MPNs). Cirrhosis of liver was observed in 74% of the patients. 8.7% of patients developed BCS after receiving the COVID-19 vaccine (Ad26.COV2.S). 91.3% of patients received long-term anticoagulation. 65% of patients received TIPS and/or liver transplant.
Conclusion: The most common primary cause of BCS in our study was MPNs (57%). Vaccine-induced thrombotic thrombocytopenia (VITT) after COVID-19 vaccine was found to be a newly described primary cause of BCS.
-

Nutritional Status and GI Symptoms in Pediatric Patients with Cystic Fibrosis
David J. Griego, Ashley Deschamp, Barbara Bice, and Diane Acquazzino
BACKGROUND: Cystic fibrosis (CF) is a genetic disorder that affects many organ systems including the lungs and the gastrointestinal tract. Children with CF often suffer from exocrine pancreatic insufficiency (EPI), causing many issues including poor digestion and poor nutrient absorption. It is imperative that children with CF consume greater amounts of calories, fat, protein, and fat-soluble vitamins to maintain healthy BMI. Studies have shown that adequate nutritional status leads to less severe symptoms and increased ability to fight off infection.
OBJECTIVE: The purpose of this study was to evaluate the nutritional intake and frequency of GI symptoms in CF participants compared to their non-CF siblings.
METHODS: Participants with CF and their siblings without CF were recruited for this study. Each participant completed a food frequency questionnaire and a GI symptom questionnaire. Data from the food frequency questionnaire was analyzed to determine the approximate composition of each food or drink that was reported. These values were then compared to published dietary reference intakes (DRIs) specific to healthy individuals and children with CF.
RESULTS: No significant difference was observed in macronutrient intake between CF and non-CF participants. Our CF participants were deficient in non-fermentable fiber (52%), vitamin A (48%), vitamin E (96%), and vitamin K (100%). CF participants consumed excessive calcium (87%), zinc (87%), sodium (87%), iron (91%), and magnesium (83%). Significant differences were observed between CF and non-CF nutrient intakes of zinc (p=0.05), iron (p=0.04), vitamin A (p=0.03), vitamin E (p=0.003), vitamin C (p=0.05), and vitamin B-12 (p=0.03). CF participants experienced more frequent GI symptoms than non-CF participants. Among CF participants, individuals with the homozygous f508del mutation experienced more frequent GI symptoms than those with the heterozygous f508del mutation.
CONCLUSIONS: All participants were eating well and meeting their macronutrient goals. Some dietary deficiencies existed in CF participants, including non-fermentable fiber, and vitamins A, E, and K. Exploring their clinical effects will be a future area of focus. GI symptoms were common in participants with CF, highlighting the need for interventions in this area. Also, GI symptoms in homozygous f508del patients were more frequent than in heterozygous f508del patients. These findings will be used in larger analyses to assess links between dietary intake and composition of the gut microbiome.
-

Role of Liver Stiffness and Alcohol on HBV Infection Pathogenesis
Tabitha Lynn Guyett, Grace Bybee, Youra Moeun, Moses New-Aaron, Srivatsan Kidambi, Natalia Osna, and Murali Ganesan
Hepatitis B Virus (HBV) is an infection that specifically targets hepatocytes and persistence of infection leads to inflammation and liver injury. The metabolism of alcohol is also known to cause injury and inflammation in the liver. The extent of liver damage can be analyzed by determining the pressure of the tissue with an ultrasound. As you go from a healthy liver to a fibrotic liver, the pressure increases from around 2 kPa to greater than 12.5 kPa. Previous studies have found that liver stiffness affects the primary hepatocyte function and cell interaction, but the exact mechanism behind the combined role of liver stiffness and alcohol in HBV infection is still unclear. This study aimed to determine the effect of liver stiffness and alcohol metabolism on HBV infection pathogenesis. To accomplish this aim, we used a soft and stiff liver model engineered specifically to a 2 kPa (healthy liver tissue) and 25 kPa pressure (fibrotic liver tissue). HBV transfected HepG2.2.15 cells were plated on these liver model plates. To mimic alcohol metabolism, the cells were exposed to Acetaldehyde Generating System (AGS). Results showed that liver stiffness significantly increased HBV infection markers and decreased the interferon alpha signaling by up regulating USP-18. In addition, liver stiffness increased inflammasome and pro-fibrotic markers in HBV transfected cells. The combination of alcohol metabolism with liver stiffness potentiated the HBV infection. We conclude that liver stiffness impairs interferon alpha signaling thereby increasing HBV persistence, which leads to liver inflammation and fibrosis. This study of the liver environment’s role in HBV infection and alcohol metabolism paves the way to new treatment options for patients as well as introduces more accurate lab models for research.
-

Investigating Immune Profiles in Differentiated Thyroid Cancer by Multiplex Immunofluorescence
Kemal Hajric; Krysten Vance BS; Ernesto Martinez-Duarte MD; Ana Yuil-Valdes MD; Michael Hollingsworth PhD; Melissa Holzapfel BS; Salma Elhag; Madelyn Fitch; Oleg Shats; Whitney Goldner MD; Apar Ganti MD; Hamid Band MD, PhD; Benjamin Swanson MD, PhD; and Anupam Kotwal MBBS
BACKGROUND: As the most common endocrine malignancy in the United States (U.S.), differentiated thyroid cancer (DTC) accounts for 3.8% of all cancers in the U.S., with roughly 10% of cases progressing to distant metastatic DTC, which is associated with a poor five year survival outcome despite conventional management, including surgery and radioactive iodine ablation. Recently, novel immunotherapies have garnered attention as a viable therapeutic resource for patients with advanced DTC. However, the response to therapy has been variable and unpredictable, which may be associated with an immune suppressive circulating phenotype. Nonetheless, the intra-tumoral immune infiltrate remains to be elucidated, demonstrating a critical need to address the gap in understanding in order to better prognosticate the disease.
OBJECTIVE: To identify and compare tumor-infiltrating immune markers with those present in the adjacent normal thyroid tissue, and collate these immune infiltrates with tumor characteristics.
METHODS: Twenty-nine adult tissue samples containing tumor and stromal regions were collected from patients with DTC. The samples were analyzed using multiplex immunofluorescence (MxIF) with antibodies against cell-surface molecules CD56, PD-1, PD-L1, FOXP3, CD3, CD8, CD4, CD45, CD68, CD163, INOS, HLA-DR, CD33, and CD19. 17 of the specimens were analyzed using HALO and a positive threshold was assigned based on review by a trained researcher.
RESULTS: In evaluating the immune profiles, important differences in the immune infiltrates between different stages of the cancer were observed. Generally, PD-1 and PD-L1 were highly expressed within the tumor, despite variability in lymphocyte infiltration, indicating the importance of PD-1 and PD-L1 as potential predictive biomarkers for the aggressiveness of thyroid cancer. Tumor from patients with distant metastases demonstrated higher T cell infiltration, T regulatory cells, macrophages and PD-L1 positive cells as compared to localized tumor.
CONCLUSION: Immune profiling demonstrated significant differences between tumor and adjacent healthy regions, particularly in terms of PD-1 and PD-L1 expression and lymphocyte infiltration, indicating that higher intratumor infiltration of T regulatory cells, macrophages and PD-1/PD-L1 positive cells may be associated with advanced thyroid cancer. Therefore, the data demonstrates the efficacy of MxIF in gathering valuable information regarding the tumor microenvironment, which will have major implications in guiding the selection of patients for immunotherapy.
-

Systematic Review of Preclinical Surgical Meshes for Hernia Repair
Andrew Hedstrom, Nathan Bills, Cynthia M. Schmidt, and Mark A. Carlson
Hernia repair is one of the most common procedures performed around the world. Surgical mesh materials are used to reinforce hernia repairs and improve surgical outcomes. However, current commercial mesh materials produce problems such as infection, rejection, shrinkage, adhesion, and mechanical failure. These problems contribute to a high rate of hernia recurrence and mesh removal. With the number of hernias expected to rise in the future due to increases in obesity and diabetes, the need for more effective mesh materials is critical. This review aims to identify, evaluate, and summarize experimental surgical mesh materials used in the preclinical stages of development and catalogue their characteristics and the tests used for their evaluation.
-

Radiogenomics: Combining SNP Studies with Pancreatic Ductal Adenocarcinoma Medical Images
Subhan Iqbal
Radiogenomics is a fusion of two methods, radiomics, and genomics. Radiomics is the process in which features are extracted from medical images such as MRIs, CT scans, and PET scans. Genomics on the other hand is studying an organism's genome and, in this study, their respective gene mutations. By combining both methods, radiogenomics can help find biomarkers for various cancers to help diagnose and treat patients more efficiently. In this study, Radiogenomics was used to find an association between genomic profiles and imaging features of patients with pancreatic ductal adenocarcinoma (PDAC). Out of a total of 117 patients available, only 29 patients were selected for the study. The study required that the patients must have a complete genetic profile available, a preoperative CT scan, PDAC, and are participating in the Rapid Autopsy Program (RAP).
-
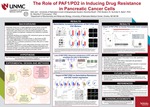
The Role of PAF1/PD2 in Inducing Drug Resistance In Pancreatic Cancer Cells
Aditi Jain, Sanchita Rauth, Surinder K. Batra, and Moorthy P. Ponnusamy
Pancreatic cancer is a highly aggressive human cancer and the third leading cause of death due to cancer. Cancer stems cells (CSC) are a small population of cancer cells that mediate tumorigenesis, metastasis, and resistance to standard treatments. By specifically identifying and targeting CSC maintenance genes, the efficiency of treatment modalities can be improved. PAF1 (RNA Polymerase II-Associated Factor 1), also known as PD2 (Pancreatic Differentiation 2) maintains pluripotency of stem cells and is a marker of pancreatic cancer stem cells. It is upregulated in poorly differentiated pancreatic cancer cells. Gemcitabine is a novel deoxycytidine analogue which has been developed as an anticancer therapy. It is widely used as a chemotherapeutic agent and is presently the most effective agent against pancreatic cancer.
Our project aimed at understanding the role of PAF1/PD2 in the maintenance of pancreatic cancer stem cells and its contribution to gemcitabine resistance. Immunohistochemistry and Bioinformatics analysis showed increased PAF1 expression in PDAC tumor samples. Through various experimental methods, it was shown that gemcitabine increases the expression of PAF1/PD2 and CSC markers and that the loss of PAF1/PD2 influences the maintenance of PC cells and sensitizes the cells to gemcitabine. The impact of PAF1/PD2 on gemcitabine resistance and CSC marker expression and on human pancreatic tumor samples was also studied.
It was concluded that PAF1/PD2 are overexpressed in pancreatic tumor cells, increased expression of PAF1/PD2 is associated with gemcitabine resistance in pancreatic cancer cells, the knockdown of PAF1/PD2 leads to a significant reduction in expression of CSC markers and pancreatic tumorigenesis, and human pancreatic tumor samples showed increased expression of PAF1/PD2. Additionally, altered expression of PAF1/PD2 has prognostic relevance to pancreatic cancer patient survival.
-

Proline biosynthesis regulates proline transport in Staphylococcus aureus.
Alyssa NL Jarabek, McKenzie K. Lehman, and Paul D. Fey
Staphylococcus aureus is metabolically diverse with the ability to rapidly adapt to a vast array of nutrient sources. This allows the pathogen to colonize a variety of niches in the host. For instance, S. aureus is the leading cause of skin and soft tissue infections, a niche that has been shown to become glucose-depleted over the course of an infection. Previous studies have shown that in niches where glucose is deficient, S. aureus utilizes peptides and free amino acids as nutrient sources. Primarily, these amino acids include glutamate and amino acids that can serve as substrates for glutamate synthesis. While arginine and histidine serve as substrates in glutamate synthesis, proline is the primary source of glutamate. Indeed, S. aureus utilizes proline as a secondary carbon source only when glucose is absent, and it can be synthesized from arginine or acquired via proline transporters from its environment. Although S. aureus encodes two putative pathways for proline biosynthesis, it has been shown that pyrroline-5-carboxylate reductase (encoded by proC) is the sole proline biosynthetic pathway in S. aureus. Studies from our laboratory have revealed that despite encoding five putative proline transporters (B7H15_03660, opuC, opuD, proP, putP), only two of the transporters, PutP and B7H15_03660 are responsible for a majority of proline transport under the laboratory conditions tested. Surprisingly, when we introduced the proC mutation into the B7H15_03660 putP double mutant, we observed proline-dependent growth, even though the primary proline transporters and proline biosynthetic pathway were knocked-out. In contrast, a transporter null ΔproC strain was unable to grow. These data suggest that inhibiting proline biosynthesis alters proline transport, and therefore one or more of the additional transporters, OpuC, OpuD, and/or ProP, are activated under these conditions. After introducing opuC, opuD, and/or proP mutations into the Δ03660 ΔputP ΔproC strain, we found that both OpuC and ProP are important for proline transport. Additionally, we observed proline-dependent growth in a proline transporter null ΔproC strain when high amounts of exogenous proline are added to the media. This growth appears to be due to an acquired mutation and will be studied more in the future. Overall these studies have revealed that proline transport is tightly linked to proline biosynthesis.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.